In a Crohn’s & Colitis UK survey, almost half of people waited a year for their diagnosis, and nearly 1 in 5 said it took over 5 years1. Having clear pathways in place not only improves the patient experience during a time when they are experiencing difficult and debilitating symptoms, but it can have an impact on the NHS, as delayed diagnosis is likely to lead to poorer prognosis and more expensive treatment options2.
Work has been carried out in recent years to improve diagnosis, including the RCGP and Crohn’s & Colitis UK IBD Spotlight Project, which aims to improve the detection and diagnosis of IBD and to support primary care clinicians to treat, manage and refer patients with Crohn’s and Colitis, but there is still more to be done.
Here we explore ‘what good looks like’ when implementing a new referral pathway and how it can lead to tangible improvements within the service and for patients.
Who's doing it well?
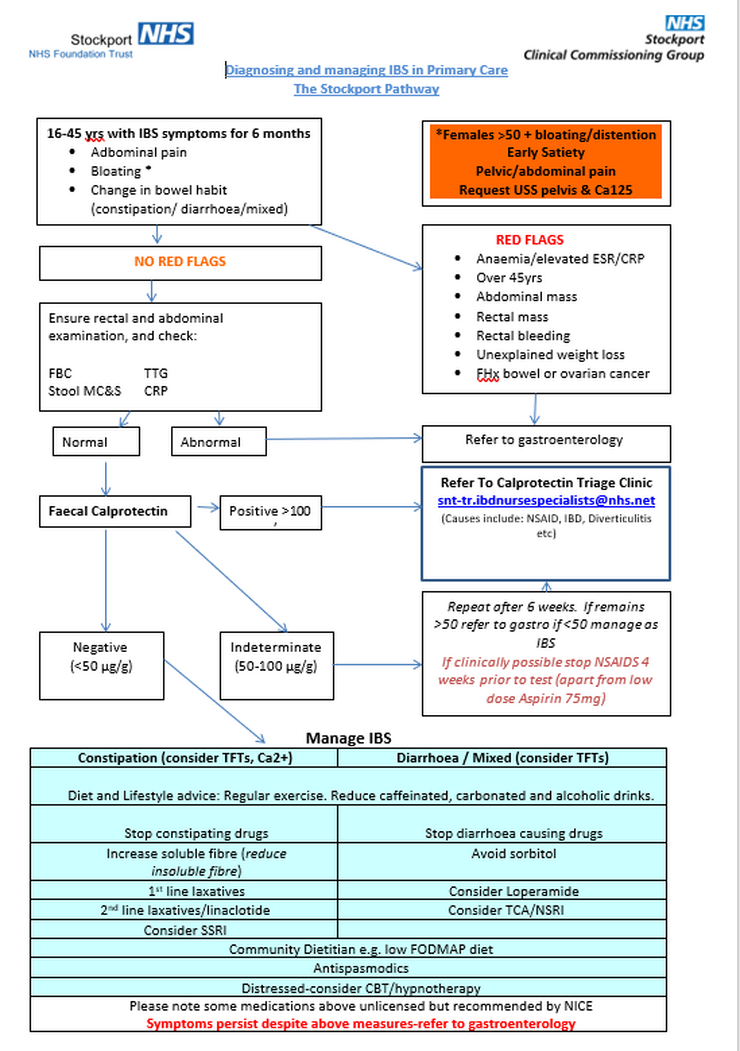
Stockport NHS Foundation Trust introduced a nurse-led raised faecal calprotectin pathway for GPs where patients with suspected IBD were referred into a new nurse clinic for assessment and diagnosis. This led to a significant reduction in time from referral to treatment for patients.
Introduced by Rachel Campbell, IBD Clinical Nurse Specialist, this case study details a retrospective examination of the IBD vs IBS referral pathway and rapid access clinic over a period of eighteen months.
The idea
There has been a recent shift in primary care to better identify suspected inflammatory bowel disease patients through pathways for referral, including the use of the biomarker faecal calprotectin. Alongside this, in May 2016, NHS England along with a local clinical commissioning group set a ‘100-day challenge’ to reduce the referral to treatment or diagnosis time for IBD to 10 weeks.
Stockport NHS Foundation Trust developed and initiated a new rapid access clinic within three weeks of the NHS challenge being set.
Once patients were reviewed by GPs using the new IBS vs IBD pathway, they received their initial clinic appointment within 7 days of referral and investigations were ordered where necessary. These patients attended the rapid access clinic and during this were physically assessed, a detailed history taken, and lifestyle examined. As this clinic was nurse-led, patients were seen by specialist nurses as the first port of call.
Results
In the period from May 2016 to January 2018, an average of 25 new patients a month were reviewed in a new patient rapid access clinic by an IBD nurse specialist (total = 400). The overall referral to diagnosis time had decreased from the previous 30+ weeks to between 8-10 weeks.
Using this pathway and rapid access clinic, 49% of patients received a diagnosis. 32% were diagnosed with Inflammatory Bowel Disease and 17% of people received a differential diagnosis, with Microscopic Colitis accounting for 12.5% of those – a diagnosis that could have potentially been missed in the past.
The IBS vs IBD pathway that was developed initially had a cut off faecal calprotectin of 50, but this meant that around 100 patients were sent in with a minimal rise (51-100) and no IBD was found on the investigations. The pathway was then revised and the cut off for faecal calprotectin was raised to 100. Now having a greater understanding of the correct cut off could mean fewer unnecessary investigations in the future.
The rapid assess clinic reduced pressure on outpatient referrals for the Gastroenterology Consultants, although adding new patients to an existing IBD Nurse Specialist workload brought some challenges. However, the benefits to patients seen in line with both NICE and IBD quality standards outweighed the pressures of the challenge.
Patients also had a much better experience – they were seen quickly and had the added value of seeing an IBD Nurse Specialist.
1Crohn’s & Colitis UK’s 2018 Survey of UK members
2Bassi A, Dodd S, Williamson P, Bodger K. Cost of illness of Inflammatory Bowel Disease in the UK: a single centre retrospective study. Gut, 2004;53(10):1471-8
Date created: May 2019