Being told you have IBD can be an incredibly stressful time. But there are clear benefits when newly diagnosed patients are well informed about their condition and how it can be treated. Not only are they in a better position to adapt to the physical, social and psychological impact of IBD, but they also show improved ability and confidence to manage their condition.
When they get their diagnosis, people should have their condition explained clearly, understand the service being offered to them and know how to access ongoing support from the IBD team. Clinicians should be prepared to repeat this information as the person comes to terms with their new diagnosis.
It’s also important to give clear written information about IBD to people at the time and place of diagnosis, which reinforces what they are being told by clinicians. This information should be appropriate to the age, understanding and communication needs of the patient and carers.
Often, people feel much more able to take in the details of their condition, and the support available, once the initial anxiety surrounding diagnosis has passed. That’s why it’s also important to share with them the many other sources of information, which they can access at their convenience.
There are lots of voluntary organisations which can support people with IBD and their carers or family, both at the point of diagnosis and afterwards. They frequently offer many valuable services, tools and support – from practical, high quality information, including packs specifically designed for people who are newly diagnosed, to helplines and local networks of people in a similar situation. They can be a highly valued source of support throughout someone’s life with IBD.
Who's doing it well?
In a survey of 150 patients at St Mark’s Hospital, London, 60% of patients perceived themselves to be well-informed about their condition yet reported low levels of knowledge on self-management during a flare. 80% expressed a wish for more information on how to manage their IBD. There was no framework to offer regular education to support shared decision making early in the disease course.
The idea
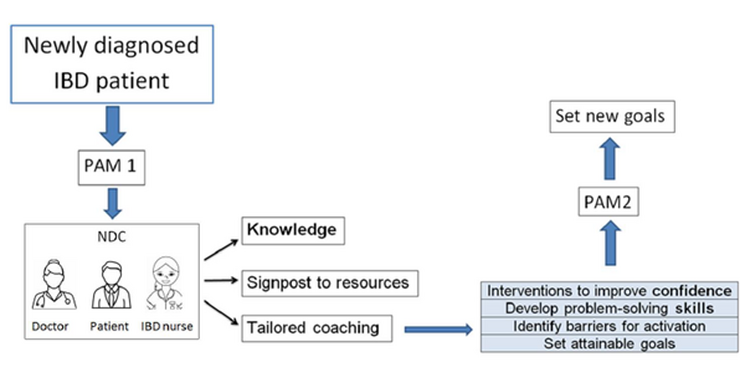
The Inflammatory Bowel Disease (IBD) team at St. Mark’s Hospital based at London North West University Healthcare Trust set up a dedicated new IBD diagnosis clinic as part of a service improvement project.
This clinic offers 45 minutes for each patient and is run by an IBD physician and an IBD nurse specialist. Patients are provided with information on self-management, surveillance of their disease activity, and reliable sources of information (Crohn’s & Colitis UK, and the St Mark’s Flare Management Card and Service Information booklet).
Results
The effectiveness of this service has been objectively assessed using the Patient Activation Measure (PAM) tool. Patient activation was measured before and after the first consultation. PAM is a validated questionnaire that measures knowledge, skills and confidence in patients and captures the extent to which people feel engaged and confident in taking care of their condition. Anxiety and depression were also assessed using the Generalised Anxiety Disorder scale and Patient Health Questionnaire at the first clinic visit.
The PAM showed that half of the patients attending the clinic had low levels of activation before the first consultation. With tailored education, 57% had an improved PAM score. Depression was also found to be a potential barrier to patient empowerment. Early assessment of patients’ activation levels and mental health was recommended to guide healthcare providers to offer individualised care.
The team are currently assessing if this level of improvement was maintained after 6 months and 12 months following their clinic attendance.